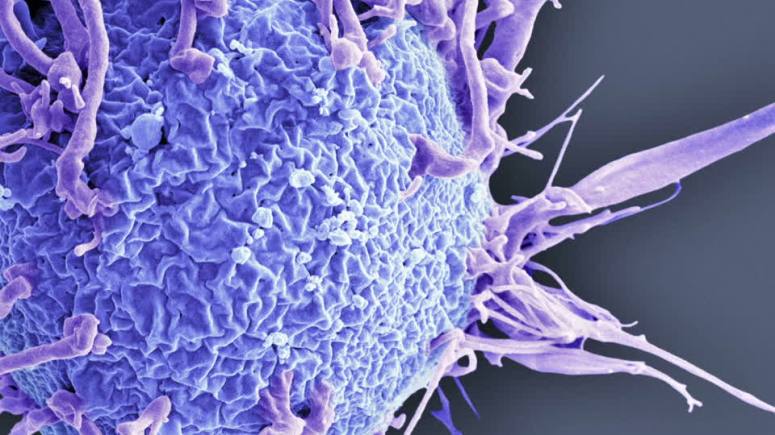
A chimeric
antigen receptor T-cell therapy targeting B-cell maturation antigen
produced high response rates with manageable toxicity among patients
with heavily pretreated relapsed or refractory multiple myeloma,
according to results of a phase 1 study. “The adverse events noted in
our study were very manageable, and we saw low rates of cytokine release
syndrome and neurotoxicity,” Noopur Raje, MD,director
of the Center for Multiple Myeloma at Massachusetts General Hospital and
professor of medicine at Harvard Medical School.
“[The
toxicity] was manageable to the extent that we are now thinking [forward
to] outpatient settings. Response rates were high, but we did not see a
plateauing of responses in very late-stage multiple myeloma.”
The CAR T-cell therapy bb2121 (Celgene, Bluebird Bio) has shown promise in preclinical studies for treatment of multiple melanoma, for which new therapies have prolonged survival but failed to prevent relapse.
Raje and
colleagues reported results from the first 33 patients (median age, 60
years, range, 37-75; men, n = 21) with relapsed or refractory multiple
myeloma who received bb2121 in the dose-escalation (n = 21) and
dose-expansion (n = 12) phases of the open-label, multicenter trial. All
patients had received at least three previous lines of therapy that
included a proteasome inhibitor and an immunomodulatory agent or were
double refractory. All patients in the dose-escalation cohort and two
patients in the dose-expansion cohort had tumor B-cell maturation
antigen (BCMA) expression of 50% or greater.
After
undergoing lymphodepletion with fludarabine and cyclophosphamide,
patients received bb2121 as a single infusion at doses of 50 x 106, 150 x 106, 450 x 106 or 800 x 106 CAR-positive T cells in the dose-escalation phase and 150 x 106 to 450 x 106 CAR-positive T cells in the expansion phase.
Safety served as the primary endpoint. Data cutoff occurred 6.2 months after the last infusion.
Results
showed an objective response rate of 85% (95% CI, 68.1-94.9), with 15
patients (45%) achieving a complete response, six of whom have since
relapsed.
Median PFS was 11.8 months (95% CI, 6.2-17.8).
Sixteen patients with partial or complete responses appeared negative for minimal residual disease ( 10-4 nucleated cells).
All 33 patients experienced adverse events, including 28 (85%) who experienced a grade 4 event.
The most
common grade 4 hematologic adverse events included neutropenia (n = 26),
leukopenia (n = 13), thrombocytopenia (n = 10) and lymphopenia (n = 9).
Grade 3 hematologic adverse events included anemia (n = 15), leukopenia
(n = 6) and thrombocytopenia (n = 5).
Get to know more about hemonc at: http://bit.ly/2xaW3zT
No comments:
Post a Comment